- India
- Dec 30
Explainer / Ayushman Bharat-Health and Wellness Centres
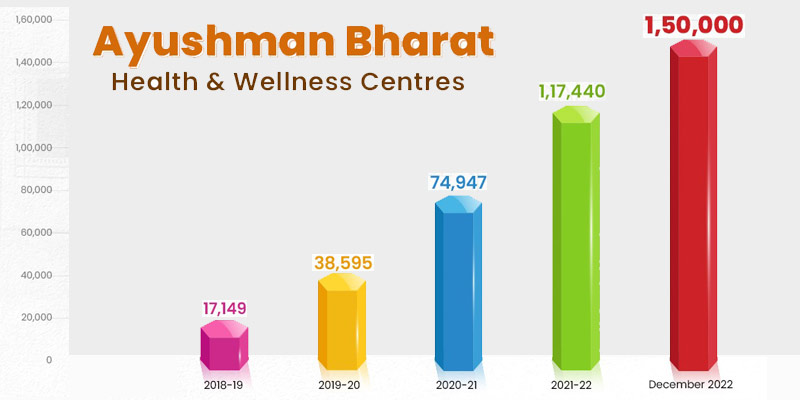
The government has achieved the target of operationalising 1.5 lakh Ayushman Bharat-Health and Wellness Centres (AB-HWCs) across the country, Health Minister Mansukh Mandaviya said.
Under the Ayushman Bharat, the government had set a target of transforming existing 150,000 lakh Sub-Health Centres (SHCs) and rural and urban Primary Health Centres (PHCs) across the country as AB-HWCs by December 2022 to bring health care closer to the community.
Ayushman Bharat
The launch of Ayushman Bharat in 2018 marked a significant landmark in the history of health in India. Ayushman Bharat is India’s road to Universal Health Care, and when fully operational will ensure universal, accessible, equitable and affordable health care for all.
It has been designed to meet Sustainable Development Goals (SDGs) and its underlying commitment, which is to “leave no one behind”.
The aim is to provide essential health services throughout the country, through the four pillars of this programme:
i) Health and Wellness Centres (HWCs)
ii) Pradhan Mantri-Jan Arogya Yojana (PM-JAY)
iii) Ayushman Bharat Digital Mission
iv) Pradhan Mantri-Ayushman Bharat Health Infrastructure Mission.
i) Health and Wellness Centres (AB-HWCs)
• The first component pertains to creation of 150,000 Health and Wellness Centres (AB-HWCs) by upgrading the Sub-Health Centres (SHCs) and Primary Health Centres (PHCs) in rural and urban areas which will bring health care closer to the community.
• These AB-HWCs will provide Comprehensive Primary Health Care (CPHC), by expanding and strengthening the existing Reproductive & Child Health (RCH) services and communicable diseases services and by including services related to non-communicable diseases, to begin with the common NCDs such as hypertension and diabetes, oral cancer, breast cancer and cervical cancer.
• It is also envisaged to incrementally add primary health care services for mental health, ENT, ophthalmology, oral health, geriatric and palliative health care and trauma care as well as health promotion and wellness activities like yoga.
• A few states/UTs have already started rolling out these additional packages of services in a phased manner.
ii) Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (AB-PMJAY)
• The second component is the Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) which provides health coverage up to Rs 5 lakh per family per year to around identified 10.74 crore poor and vulnerable families identified based on Socio Economic Caste Census (SECC) data.
• The out-of-pocket expenditure for hospitalisation pushes millions of people into poverty every year. In order to address this and provide health cover of Rs 5 lakh per family per year for secondary and tertiary care hospitalisation to poor and vulnerable section of the population, AB-PMJAY was launched, subsuming the erstwhile Rashtriya Swasthya Bima Yojana, in September 2018.
• The scheme aims to improve affordability, accessibility, and quality of care for the poor and vulnerable section of the population.
• Ayushman Bharat marks a paradigm shift to move from a sectoral and selective approach of health service delivery to a comprehensive range of health care services. Ayushman Bharat aims to holistically address health (covering prevention, promotion and ambulatory care), at primary, secondary and tertiary level by adopting a continuum of care approach.
• This health cover includes 3 days of pre-hospitalisation and 15 days of post-hospitalisation expenses.
• There is no cap on family size, age or gender to ensure that all members of the beneficiary families are covered. Also, benefits are portable across the country.
• Services include approximately a range of procedures covering all the costs related to treatment, including but not limited to drugs, supplies, diagnostic services, physician’s fees, room charges, surgeon charges, OT and ICU charges, etc.
• AB-PMJAY is an entitlement-based scheme. Eligible beneficiaries can directly visit any empanelled public or private hospital to avail cashless treatment.
• The beneficiaries will not be required to pay any charges for the hospitalisation expenses.
• Ayushman cards are issued to the beneficiaries to create awareness about the scheme.
• States/UTs have the flexibility to run their own health protection schemes in alliance with AB-PMJAY at their own cost. Accordingly, states/UTs have expanded the scheme coverage to 14.75 crore beneficiary families at their own cost.
• The funding of the scheme is shared between central and state governments. The ratio of central share to state share for all states, except northeast states and Himalayan states and Union Territories with legislature, is 60:40. For northeast states and Himalayan states, the ratio is 90:10. In the case of Union Territories without legislatures, the central contribution of premium is 100 per cent.
How is AB-PMJAY implemented?
• At the central level, National Health Authority (NHA) has been set up as an attached office to the ministry of health and family welfare for implementing AB-PMJAY.
• NHA is headed by a full time CEO in the rank of secretary to the government of India. An 11 member Governing Board (GB), headed by the minister for health has also been established as the decision making body of the NHA.
• State Health Agency (SHA) is the nodal agency responsible for implementation of AB-PMJAY in the state. In addition to the state level posts, District Implementation Units (DIUs) have also been set up to support the implementation in districts.
• National Health Authority (NHA) has launched the new version of Health Benefit Package (HBP) 2022 under the AB PM-JAY scheme. The new version has added 365 new procedures taking the total package count to 1,949. With HBP 2022, differential pricing is being introduced for the first time under the scheme based upon the type of city and level of care.
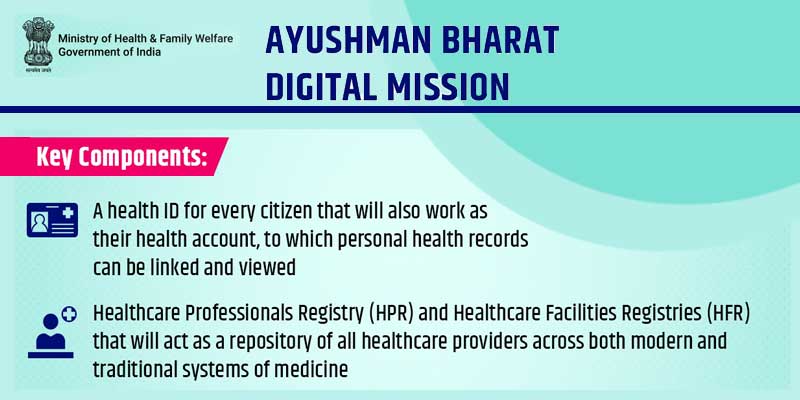
iii) Ayushman Bharat Digital Mission
• In September 2021, Prime Minister Narendra Modi launched the Ayushman Bharat Digital Mission (ABDM).
• It was originally called the National Digital Health Mission and launched on August 15, 2020 as a pilot in six Union Territories.
• Based on the foundations laid down in the form of Jan Dhan, Aadhaar and Mobile (JAM) trinity and other digital initiatives of the government, Ayushman Bharat Digital Mission (ABDM) is creating a seamless online platform through the provision of a wide-range of data, information and infrastructure services, duly leveraging open, interoperable, standards-based digital systems while ensuring the security, confidentiality and privacy of health-related personal information.
• Citizens will only be a click away from accessing health care facilities.
• Under the mission, citizens will get a digital health ID.
iv) Pradhan Mantri-Ayushman Bharat Health Infrastructure Mission
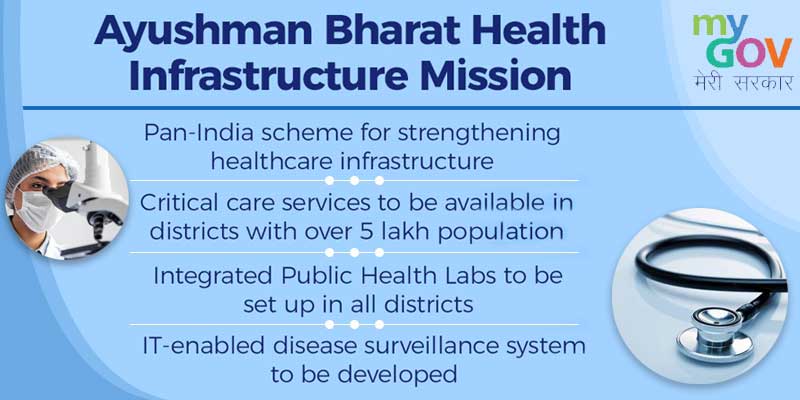
• Pradhan Mantri-Ayushman Bharat Health Infrastructure Mission is one of the largest pan-India schemes for strengthening health care infrastructure across the country. It is in addition to the National Health Mission.
• Its objective is to fill gaps in public health infrastructure, especially in critical care facilities and primary care in both urban and rural areas.
• It will provide support for 17,788 rural health and wellness centres in 10 high focus states. Further, 11,024 urban health and wellness centres will be established in all the states.
• Through this, critical care services will be available in all the districts of the country with more than five lakh population through exclusive critical care hospital blocks, while the remaining districts will be covered through referral services.
• People will have access to a full range of diagnostic services in the public healthcare system through a network of laboratories across the country, and integrated public health labs will be set up in all the districts.
Manorama Yearbook app is now available on Google Play Store and iOS App Store