- India
- Jan 14
Odisha joins Ayushman Bharat-PMJAY scheme
• Odisha became the 34th state to implement the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY).
• The National Health Authority (NHA) signed the MoU with Odisha government’s health and family welfare department at the Vigyan Bhavan in the presence of Union Health Minister J.P. Nadda and Odisha Chief Minister Mohan Charan Majhi.
• The scheme will be implemented in convergence with the existing Gopabandhu Jan Arogya Yojana (GJAY) in Odisha. It will provide a cover of Rs 5 lakh per family per annum with an additional Rs 5 lakh for women members.
• Approximately 1.03 crore families will come under the converged scheme with the Union government supporting 67.8 lakh of them.
Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (AB-PMJAY)
• Over the past few decades there has been improvement in various health indicators of India. However, the out-of-pocket expenditure, which pushes millions of people into poverty every year.
• In order to address this and provide health cover of Rs 5 lakh per family per year for secondary and tertiary care hospitalisation to poor and vulnerable section of the population, Ayushman Bharat–Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) was launched, subsuming the erstwhile Rashtriya Swasthya Bima Yojana, on September 23, 2018.
• It is the largest publicly funded health assurance scheme in the world.
• AB-PMJAY scheme has witnessed continuous expansion of the beneficiary base.
• Initially, 10.74 crore poor and vulnerable families comprising the bottom 40 per cent of India's population were covered under the scheme.
• In January 2022, the Union government revised the beneficiary base from 10.74 crore to 12 crore families considering India's decadal population growth of 11.7 per cent over the 2011 population.
• The scheme was further expanded to cover 37 lakh ASHAs/AWWs/AWHs working across the country and their families for free healthcare benefits.
• Currently, 55 crore individuals corresponding to 12.34 crore families are covered under the scheme. Further, many states have expanded beneficiary base on their own.
• The scheme is implemented in 34 states/UTs except the NCT of Delhi and West Bengal.
• All members of the eligible families irrespective of age are covered under the scheme.
• The funding of the scheme is shared between central and state governments. The ratio of central share to state share for all states except northeast states and Himalayan states and Union Territories with legislature, is 60:40. For northeast states and Himalayan states, the ratio is 90:10. In the case of Union Territories without legislatures, the central contribution of premium is 100 per cent.
Features of AB-PMJAY:
• The AB-PMJAY scheme is completely cashless and paperless and without the concept of reimbursement. Beneficiaries can avail treatment under defined packages.
• It is an entitlement-based scheme. Eligible beneficiaries can directly visit any empanelled public or private hospital to avail cashless treatment. Ayushman cards are issued to the beneficiaries to create awareness about the scheme.
• As of June 30, 2024, more than 34.7 crore Ayushman cards have been created under the scheme in the country.
• The Empanelled Healthcare Providers are paid based on specified health benefit packages with standardised rates.
• The scheme has covered 8.19 crore hospital admissions, including 49 per cent women beneficiaries. The public has benefited to the extent of over Rs 1.13 lakh crore under the scheme, the government said.
• Nearly 2,000 medical procedures across 27 specialties are covered under AB-PMJAY, including major surgeries like bypass surgeries and knee replacements.
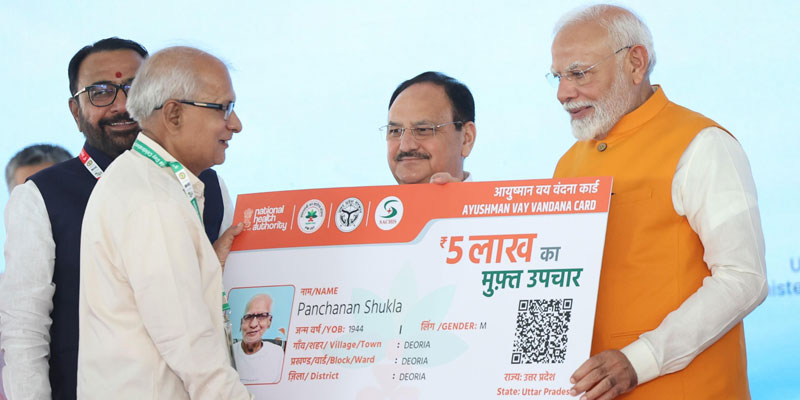
Expansion of health coverage to all persons aged 70 years and above
• In October 2024, the Union government announced the expansion of Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) to include all people aged 70 years and above.
• Under the expansion, all people aged 70 years and above will receive ‘Ayushman Vay Vandana Card’ which will help them avail healthcare benefits.
• The Rs 5 lakh free health insurance cover would benefit approximately six crore senior citizens of around 4.5 crore families.
• Ayushman Vay Vandana Card provides Rs 5 lakh free health cover to all people of the age 70 years and above irrespective of their socio-economic status.
• The senior citizens of the age 70 years and above belonging to families already covered under AB-PMJAY get an additional top-up cover up to Rs 5 lakh per year for themselves.
• Senior citizens who are already availing benefits of various government schemes including Central Government Health Scheme (CGHS), Ex-Servicemen Contributory Health Scheme (ECHS), and Ayushman Central Armed Police Force (CAPF) have to choose between their existing scheme or can opt for AB-PMJAY.
• Additionally, persons covered by private health insurance coverage or members of the Employees' State Insurance scheme are eligible to benefit from AB-PMJAY.
• The card offers treatment for around 2,000 medical procedures and covers all pre-existing diseases from the first day itself without any waiting period.
Manorama Yearbook app is now available on Google Play Store and iOS App Store