- India
- Dec 14
Scope and challenges of public health surveillance in India
• Government think tank NITI Aayog has proposed setting up a Surveillance Information Platform to strengthen India’s public health surveillance system.
• NITI Aayog released a white paper ‘Vision 2035: Public Health Surveillance in India’ on December 14.
• It envisions integration within the three-tiered health system, strengthened community based surveillance, expanded referral networks and enhanced laboratory capacity. The electronic health record (EHR) will become the main basis of surveillance and is complemented by periodic national/state/district level surveys, special studies and research in order to reconcile the threshold and redefine standard definitions of cases, as disease patterns evolve.
Public health surveillance in India
• Surveillance is ‘information for action’. Public health surveillance, an important public health function, cuts across primary, secondary and tertiary levels of health care.
• During the 1988 Cholera outbreak in Delhi and 1994 plague outbreak in Surat, with huge morbidity and mortality, the country sustained huge economic losses. This prompted the central government to constitute a National Apical Advisory Committee (NAAC) in 1995 for national disease surveillance and response system.
• In 1997, the National Surveillance Programme for Communicable Diseases was launched.
• HIV Sentinel Surveillance (HSS) was perhaps one of the first nationwide disease surveillance programmes, which began in 1992 and later expanded across the country in 1998.
Integrated Disease Surveillance Project (IDSP)
• The World Bank funded the Centre in 2004 for a ten year ‘Integrated Disease Surveillance Project (IDSP)’. This was later converted into a programme and funded under the 12th Five-year Plan (2012-17) within the National Health Mission.
The intent of the programme is:
• To detect early warning signals of impending outbreaks.
• To help initiate an effective response in a timely manner.
• To provide essential data to monitor progress of on-going disease control programmes.
• To help allocate health resources more efficiently.
• There is a list of more than 33 acute conditions covered under the IDSP.
• The IDSP has successfully integrated data from the Vector Borne Disease Control Programme including data on malaria, filariasis, dengue fever, Japanese encephalitis, chikungunya and Kyasanur Forest Disease among others.
• Other programmes such as the Diarrhoeal Disease Control Programme, zoonotic infections (rabies/dog bite and snake bite), Vaccine Preventable Diseases and Acute Respiratory Infections are also included.
• However, vertical programmes including the National AIDS Control Programme (NACP), the recently renamed National TB Elimination Programme (NTEP) and the Reproductive and Child Health (RCH) programme are not yet fully integrated into the IDSP as it took a conscious decision to focus on ‘early warning signals’ for acute conditions, leaving the large vertical national programmes to manage their own systems of surveillance.
Three levels of disease surveillance
Surveillance activities in India are organised at three levels: national, state and district.
Central Surveillance Unit (CSU)
CSU is integrated administratively and financially with the National Centre for Disease Control (NCDC), New Delhi and established by the ministry of health and family welfare for the Global Health Security Agenda (GHSA). The CSU has 14 technical centres/divisions, including epidemiology, microbiology, zoonosis, medical entomology and vector management, IDSP, Centre for AIDS and Related Diseases, biochemical and toxicology, biotechnology, parasitic diseases, malariology and coordination, occupational and environmental health, noncommunicable diseases, statistics and M&E, planning, budget and administration.
State Surveillance Unit (SSU)
There is an SSU in each state/UT with a regular officer identified as State Surveillance Officer (SSO). The SSO is supported by seven contractual staff who include training, finance, data managers, epidemiologist, microbiologist, entomologist and a recently included veterinary consultant.
District Surveillance Unit (DSU)
One in each district with a regular officer as District Surveillance Officer (DSO), supported by three contractual staff.
• In 2019, the World Health Organisation (WHO) in partnership with the Centre launched the Integrated Health Information Platform (IHIP) within the IDSP programme. The IHIP is a digital web-based open platform that captures individualised data in almost real-time, generates weekly and monthly reports of epidemic outbreaks and early warning signs and captures response by ‘rapid response teams’, for 33+ disease conditions.
• Other data sources capture information on diseases of national importance such as TB. TB was made a notifiable disease in 2012 and the Nikshay platform serves as a source of data to estimate burden and to track disease trends and outcomes.
The role of ICMR in health surveillance
• The Indian Council of Medical Research (ICMR) has played a key role in strengthening surveillance and research related to surveillance.
• The network of ICMR continues to expand and at present has 106 Viral Research and Diagnostic Laboratories (VRDL), 35 diagnostic centres and a number of apex institutions. Together, these institutions have played key roles in the identification of existing and new pathogens and their variants, in controlling newly emerging infections (SARS, Nipah virus, etc.) and in estimating disease burden using mathematical modelling for diseases like malaria and dengue fever.
• Over the years, these various institutions, networks and programmes have been fairly effective. Smallpox was eradicated in India in 1979, a year before its global eradication.
• India was declared ‘polio-free’ in 2014, three years after the last case detection in India in 2011. Epidemics of SARS, Nipah and rotavirus have been rapidly detected through the efficient viral research and diagnostic laboratory network of ICMR, and have been effectively controlled.
• The ICMR network is playing a critical role in the containment of the COVID-19 pandemic.
Challenges in India’s existing public health surveillance
• Despite significant progress and potential for an expanded and enhanced public health surveillance system in India, there are a number of challenges that need to be addressed in the short term:
1) Implementation challenges – patchy surveillance, not comprehensive: The Integrated Health Information Platform (IHIP) is not yet fully operational across the country. There are a number of notable implementation challenges. One of the important system design issues is that data on the citizen utilisation of services for treatment of disease is separate from notification mechanisms for disease outbreaks. There is a lack of uniformity in outbreak investigation and reporting and there are limitations in geographic coverage within states.
2) Surveillance functions in vertical silos of programmes and institutions: Vertical programmes such as the National AIDS Control Programme and the National TB Elimination Programme have achieved significant success in reducing disease transmission. However, surveillance data from vertical programmes are not yet fully integrated within a single unified surveillance platform.
3) Private sector involvement in surveillance is limited: The private sector is not a homogenous entity. It includes unregistered practitioners, stand-alone clinics, pharmacies and laboratories, smaller nursing homes, medium to large hospitals, medical colleges, corporate institutions and apex institutions. Additionally, there is also an entire segment of not-for-profit institutions that are run by different mission hospitals and trusts that are also included within the private sector. Private sector participation in disease surveillance is minimal.
4) Inadequate linkage of morbidity with mortality data: The Reproductive and Child Health (RCH) programme has recently begun focusing on enhancing maternal and neonatal death review to enable the identification of contributing factors and potential solutions to inform health care service deliveries and prevent future deaths. However, maternal, neonatal and child death surveillance and linking of mortality with morbidity reports is not yet fully integrated.
5) Human resource challenges: The recruitment of human resources for state and district-level surveillance units has been devolved to states, however, the response of states to address these human resource gaps is varied. Health is a state subject, while health surveillance is a national prerogative. Human resource vacancies and staff capacity continue to plague the system.
6) Training of public health core-capacity: There are many examples of training programmes for public health professionals specifically in the area of surveillance. India lacks sufficient public health experts with expertise (Masters in Public Health, Epidemic Intelligence Service – MPH-EIS).
7) Limited use of digital, social and print media in surveillance: Social and print media are increasingly being piloted for use in surveillance. A few states in the country do have operational media scanning cells or media-advocacy initiatives that help highlight disease outbreaks, or help identify a sudden increase in hospitalisation or death due to an unusual event. These media sources can also be used to promote disease prevention and containment actions at community-level during new infectious disease outbreaks.
8) Limited focus on non-communicable disease surveillance: Non-communicable disease (NCD) surveillance was introduced in many developed countries almost 35-40 years ago. India faces the dual burden of non-communicable and communicable diseases. Full integration of surveillance for NCD risk factors, disease and death statistics, and surveillance of injury and accidents, air pollution and its effects, etc are yet to be included into surveillance.
9) Fragmented and minimalistic approach in occupational health surveillance: Occupational Health Surveillance in India falls into two broad categories: Hazard surveillance and health surveillance. Despite progress and availability of occupational health data, occupational health surveillance is not a core component of India’s public health surveillance.
NITI Aayog’s vision document
• The NITI Aayog (National Institution for Transforming India - Policy Commission) was established in 2015 by the government of India as a policy think tank. Its aim is to achieve sustainable development goals through cooperative federalism, fostering the involvement of state governments and using a bottoms-up approach.
• Traditional public health disease surveillance systems in India have remained fragmented, siloed, and limited to few diseases. As India reimagines and reforms its health systems, the country needs to ensure that our public health surveillance systems are also made citizen-centric and within the context of the overall socio-economic development of the country.
• In 2020, the NITI Aayog signed a Letter of Agreement with the University of Manitoba in Canada to develop a working paper on a ‘Vision for Public Health Surveillance in India by 2035’.
• This vision document, which takes forward the vision as envisaged in the National Health Policy 2017, lays the foundation for integrated surveillance of both communicable and non-communicable diseases.
Four building blocks are envisaged for this vision:
1. An interdependent federated system of governance architecture between the Centre and states.
2. Enhanced use of new data collection and sharing mechanisms for surveillance based on unitised, citizen-centric comprehensive electronic health records (EHR) with a unique health identifier (UHID). Existing disease surveillance data and information from periodic surveys will complement this information.
3. Enhanced use of new data analytics, data science, artificial intelligence, and machine learning.
4. Advanced health informatics.
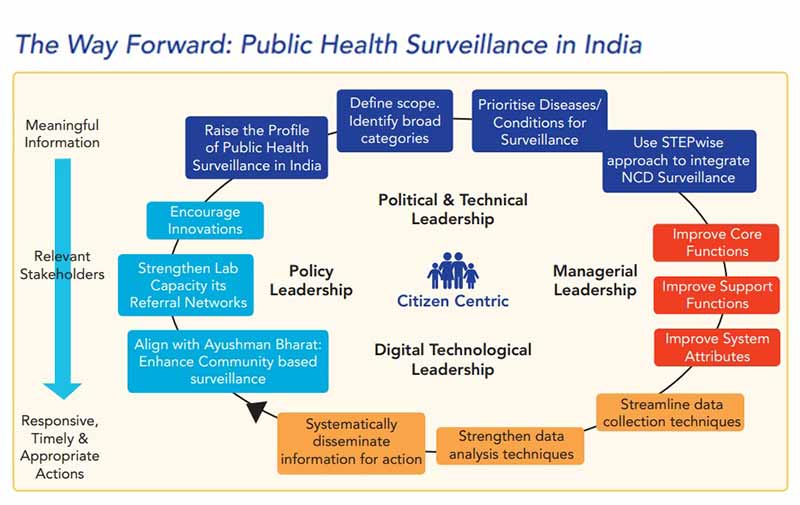
• Drawing on best practices from India and other developing and developed country experiences, the white paper suggests seven steps for India to move forward towards this vision. All these steps are in alignment with the principle to raise the profile of surveillance as a tool for the public good. The steps are suggested as a continuous cycle rather than a sequential process.
1. Establish a governance framework that is inclusive of political, policy, technical and managerial leadership at the national and state level.
2. Identify broad disease categories that will be included under public health surveillance.
3. Enhance surveillance of non-communicable diseases and conditions in a STEPwise manner.
4. Prioritise diseases that can be targeted for elimination as a public health problem, regularly.
5. Improve core support functions, core functions, and system attributes for surveillance at all levels — national, state, district and block.
6. Establish mechanisms to streamline data sharing, capture, analysis, and dissemination for action. These could include the use of situation-aware real-time signals from social media, mobile sensor networks, and participatory surveillance systems for event based epidemic intelligence.
7. Encourage innovations at every step-in surveillance activity.
The need for Surveillance Information Platform
• A Surveillance Information Platform will store, analyse, and auto-generate relevant reports for action. As well, this remains a repository for further analysis and research which will complement the available surveillance information.
• Surveillance itself functions on a single Surveillance Information Platform that amalgamates all relevant information from multiple sources. Initially, this information can come from existing vertical and integrated disease surveillance programmes.
• However, over time, this would be primarily driven from electronic health records (EHR) of populations and medical records of patients, that are individualised and identified through the use of a unique health identifier (UHID).
• Information from vertical and integrated disease control programmes, hospitals and health centres, laboratories and pharmacies, insurance related routine medical check-up, Pradhan Mantri Jan Arogya Yojana (PMJAY) and other insurance records, and occupational health surveillance will all be amalgamated into the EHR.
• In alignment with the principal of ‘one-health’ environmental health surveillance, plant and animal disease surveillance will also be integrated into this Surveillance Information Platform.
• National surveys, special studies and research will be used periodically to validate case definitions and to address gaps within the electronic health record-based surveillance.
Manorama Yearbook app is now available on Google Play Store and iOS App Store